Childhood allergies, including food allergies, asthma, and eczema, can be a significant concern for parents. A childhood allergy assessment is an important step in identifying these conditions early. Early detection and proper management are essential to helping children lead healthy, active lives without the challenges of allergies.
Doctors use many tools to check for allergies in kids. These include skin tests, blood tests, and food challenges. Each test helps find out what triggers a child’s allergic reactions. This information guides treatment plans and helps families avoid allergens.
Recent advances in allergy testing have made it easier to pinpoint specific triggers. New methods like component-resolved diagnostics offer more detailed results. These tests help doctors create better treatment plans for each child’s needs.
Overview of Childhood Allergies
Childhood allergies are common health issues that affect many kids. They happen when a child’s immune system reacts to things that are usually harmless. These reactions can range from mild to severe.
Defining Allergy and Immunology
An allergy is when the body’s immune system overreacts to a substance. This substance is called an allergen. The immune system makes antibodies to fight the allergen. This causes symptoms like sneezing, itching, or rashes.
Immunology is the study of the immune system. It looks at how the body fights off germs and other harmful things. In allergies, the immune system mistakes harmless things for threats.
Allergic reactions can affect different parts of the body. They may involve the skin, nose, eyes, lungs, or stomach.
Prevalence of Childhood Allergies
Childhood allergies are becoming more common. About 1 in 13 children have food allergies. Asthma affects around 1 in 12 kids.
Some allergies are more common in certain age groups. For example:
- Milk and egg allergies often start in babies
- Peanut allergies usually begin in toddlers
- Hay fever tends to develop in school-age children
Boys are more likely to have allergies than girls. This gap narrows as kids get older.
Common Allergens and Triggers
Many things can cause allergic reactions in children. Some of the most common include:
- Foods: peanuts, tree nuts, milk, eggs, soy, wheat
- Pollen from trees, grasses, and weeds
- Pet dander from cats, dogs, and other animals
- Dust mites
- Mold spores
- Insect stings or bites
Some kids are allergic to medicines like penicillin. Others react to latex or certain metals.
Allergic triggers can change as a child grows. A baby might outgrow a milk allergy. But they could develop new allergies later on.
Childhood Allergy Screening
Doctors use allergy screening to check if a child has allergies. These tests help find out what causes allergic reactions in kids. They also show how bad the allergy is.
Indications for Allergy Screening
Doctors might suggest allergy screening if a child has certain signs. These can include:
- Skin rashes or hives
- Breathing problems
- Runny nose or sneezing
- Stomach issues after eating
- Bad reactions to insect stings
Kids with a family history of allergies may need screening too. This is because allergies often run in families.
Screening and Diagnosis Overview
There are many ways to screen for allergies in children. Common tests include:
- Skin prick tests
- Blood tests
- Patch tests
- Food challenges
Skin prick tests put small amounts of allergens on the skin. If a red bump shows up, it means the child may be allergic. Blood tests look for special proteins in the blood that show allergies.
Patch tests help find skin allergies. Food challenges involve eating small amounts of foods to see if they cause reactions. Doctors pick the best test based on the child’s symptoms and health history.
Common Allergic Conditions in Children
Allergic conditions often start in childhood. These can affect a child’s skin, breathing, and overall health. Early diagnosis and proper management are key to improving quality of life.
Atopic Dermatitis (Eczema)
Eczema causes dry, itchy, and inflamed skin. It often shows up in babies and young children. Common spots include the face, hands, and skin folds.
Triggers can include:
- Certain foods
- Irritants like soaps
- Stress
- Dry weather
Treatment focuses on keeping skin moisturized and managing flare-ups. Doctors may suggest:
- Gentle skincare routines
- Topical medications
- Identifying and avoiding triggers
- Natural Bar of Soap
Asthma
Asthma makes breathing hard. It can cause wheezing, coughing, and chest tightness. Asthma often starts in childhood.
Triggers vary but may include:
- Allergens like pollen or dust
- Exercise
- Cold air
- Respiratory infections
Managing asthma involves:
- Using inhalers as prescribed
- Avoiding triggers
- Regular check-ups
- Having an action plan for flare-ups
Allergic Rhinitis
This condition affects the nose. It’s often called hay fever. Symptoms include:
- Sneezing
- Runny or stuffy nose
- Itchy eyes, nose, and throat
Common triggers are:
- Pollen
- Dust mites
- Pet dander
- Mold spores
Treatment may include:
- Antihistamines
- Nasal sprays
- Avoiding triggers
- Allergy shots, in some cases
Food Allergies
Food allergies can cause mild to severe reactions. Common food allergens in kids include:
- Milk
- Eggs
- Peanuts
- Tree nuts
- Soy
- Wheat
- Fish
- Shellfish
Symptoms range from hives to life-threatening anaphylaxis. Management involves:
- Strict avoidance of trigger foods
- Reading food labels carefully
- Having an emergency action plan
- Carrying epinephrine auto-injectors if prescribed
Insect Sting Allergies
Some children are allergic to insect stings. Common culprits are:
- Bees
- Wasps
- Hornets
- Fire ants
Reactions can be local or systemic. Severe allergies may cause anaphylaxis.
Prevention and treatment include:
- Avoiding insects when possible
- Wearing protective clothing outdoors
- Having an emergency action plan
- Carrying epinephrine if prescribed
- Considering venom immunotherapy for severe allergies
Drug Allergies
Drug allergies in children can be serious. Common triggers include:
- Antibiotics (like penicillin)
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Anticonvulsants
Symptoms vary from rashes to severe reactions. Management involves:
- Identifying and avoiding trigger drugs
- Using alternative medications
- Wearing medical alert jewelry
- Having an emergency action plan
In some cases, drug desensitization may be an option under medical supervision.
Diagnostic Tests
Doctors use several tests to find out what causes allergies in children. These tests help figure out which things trigger reactions and how severe they might be.
Skin Prick Test (SPT)
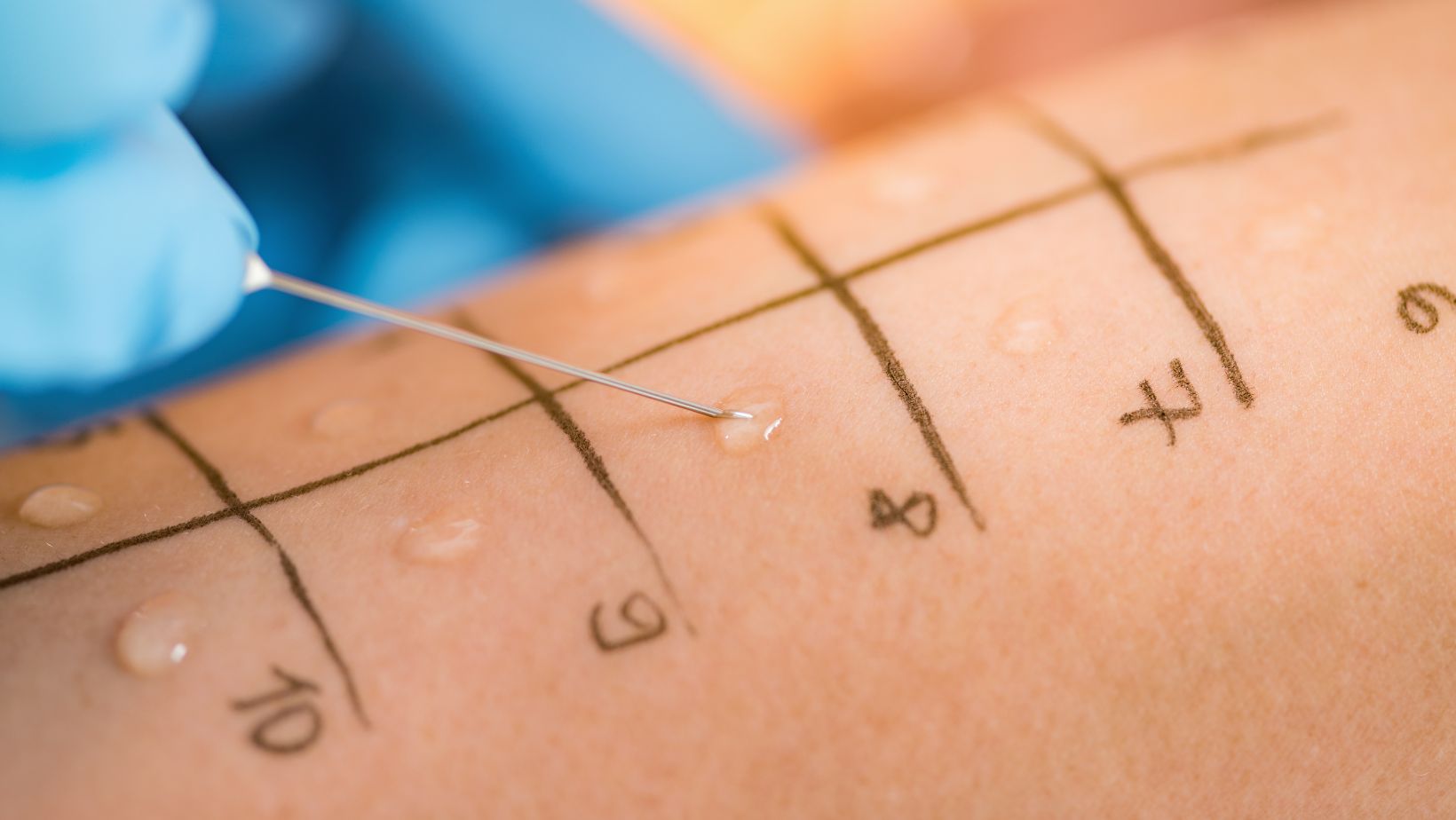
The skin prick test is a quick way to check for allergies. A doctor puts tiny amounts of possible allergens on the skin, usually on the arm or back. They then prick the skin lightly with a small needle. If a red bump shows up, it means the child might be allergic to that substance.
This test is safe and doesn’t hurt much. It can test for many allergens at once. Results show up fast, often within 15-20 minutes.
Patch Testing
Patch tests check for delayed allergic reactions. They’re good for finding contact allergies that cause skin rashes. A doctor puts small patches with allergens on the skin, usually on the back. The patches stay on for 48 hours.
The patient comes back after 2-4 days. The doctor then checks for any skin reactions. This test helps find things that might cause eczema or other skin problems.
Blood Tests (Specific IgE Testing)
Blood tests look for specific antibodies in the blood. These antibodies are called Immunoglobulin E (IgE). They show up when the body reacts to allergens. The test measures how much IgE is in the blood for each allergen.

This test is good for kids who can’t have skin tests. It’s also useful when skin tests might be dangerous. Results take a few days to come back from the lab.
Oral Food Challenge
An oral food challenge is the most accurate way to test for food allergies. The child eats small amounts of a suspected food allergen. A doctor watches closely for any reactions. The amount of food increases slowly over time.
This test is done in a medical setting. It’s important because it can show if a child has outgrown a food allergy. It can also confirm an allergy if other tests are unclear.
Elimination Diet
An elimination diet helps find food allergies or intolerances. It involves removing suspected foods from the diet for a set time. Then, these foods are added back one at a time. This helps see which foods cause symptoms.
This method takes time and careful tracking. It’s often used with other tests to get a clear picture. A doctor or dietitian should always guide an elimination diet.
Component-Resolved Diagnostics (CRD)
CRD is a newer, more detailed blood test. It looks at specific proteins in allergens. This test can tell which parts of a food or substance cause an allergy. It helps predict how severe an allergy might be.
CRD is useful for complex cases. It can show if a child might react to similar foods. This information helps doctors give more precise advice about what to avoid.
Nasal Smear Or Nasal Cytology
A nasal smear checks for cells in the nose. It can show if allergies are causing nasal symptoms. The doctor takes a sample from inside the nose with a small brush or swab. They look at the sample under a microscope.
This test can find specific types of cells linked to allergies. It helps tell the difference between allergies and other nose problems, like infections.
Spirometry
Spirometry measures how well the lungs work. It’s important for checking asthma. The child breathes into a machine called a spirometer. The test shows how much air they can breathe out and how fast.
Doctors often do this test before and after giving asthma medicine. This helps see if the medicine works. Spirometry can also show how severe asthma is.
Fractional Exhaled Nitric Oxide (FeNO) Test
The FeNO test measures nitric oxide in breath. Higher levels can mean there’s inflammation in the airways. This often happens with allergic asthma. The child breathes into a small handheld device.
This test is quick and easy. It helps doctors decide on asthma treatment. It can also show if asthma medicines are working well.
Challenge Tests
Challenge tests check how the body reacts to specific triggers. These might be foods, drugs, or things in the air. The test is done in a controlled medical setting. The child is given small amounts of the suspected allergen.
Doctors watch closely for any reactions. These tests are very helpful but can be risky. They’re only done when other tests don’t give clear answers.
Provocation Testing
Provocation tests are similar to challenge tests. They’re used to check for reactions to things like exercise or cold air. The child does an activity or is exposed to a trigger. Doctors then check for symptoms.
These tests help figure out what causes asthma attacks or other allergy symptoms. They’re done carefully to keep the child safe.
Environmental Allergen Testing
This testing checks for allergens in the child’s surroundings. It can be done at home or school. Samples are taken from the air, dust, or surfaces. These are then tested for common allergens like dust mites or mold.
The results help create a plan to reduce allergens. This can involve changes to the home or advice on avoiding triggers. It’s an important step in managing allergies in the long term.
Therapeutic Interventions
Treating childhood allergies involves several approaches. These include medications, immunotherapy, avoiding triggers, managing diet, and having emergency plans. The right mix of treatments depends on the specific allergy and its severity.
Medical Treatments and Medications
Doctors often prescribe medicines to control allergy symptoms. Antihistamines help reduce itching, sneezing, and runny nose. They come in pills, liquids, or nasal sprays.
Decongestants can relieve stuffy noses. Doctors may suggest these for short-term use.
For skin allergies, topical corticosteroids can ease itching and swelling. These creams or ointments are applied directly to the skin.
Inhaled corticosteroids are key for managing asthma. They reduce airway inflammation and help prevent attacks.
For severe allergic reactions, epinephrine auto-injectors are crucial. They quickly reverse anaphylaxis symptoms.
Allergen Immunotherapy
This treatment aims to reduce sensitivity to specific allergens over time. It involves giving small, increasing doses of an allergen.
Subcutaneous immunotherapy (SCIT) uses injections. Patients get shots at a doctor’s office every few weeks.
Sublingual immunotherapy (SLIT) uses drops or tablets under the tongue. Patients can take these at home daily.
Both methods can significantly reduce allergy symptoms. They may even prevent new allergies from developing.
Immunotherapy often lasts 3-5 years. It can provide long-lasting relief for many patients.
Environmental Control and Avoidance Strategies
Reducing exposure to allergens is a key part of allergy management. For indoor allergens like dust mites, using special bedding covers can help.
Regular cleaning with a HEPA vacuum can reduce allergens in carpets and furniture.
For pollen allergies, staying indoors on high-pollen days is helpful. Using air purifiers can improve indoor air quality.
Removing shoes before entering the house can reduce tracked-in allergens.
For pet allergies, keeping pets out of bedrooms can create an allergen-free zone for sleeping.
Dietary Management in Food Allergies
Strict avoidance of problem foods is crucial for food allergies. This requires careful label reading and asking about ingredients when eating out.
Nutritionists can help ensure a balanced diet despite food restrictions. They may suggest safe alternatives to common allergens.
Some children outgrow food allergies. Doctors may recommend periodic testing to check if this has occurred.
For mild allergies, doctors might suggest an oral immunotherapy approach. This involves eating tiny amounts of the allergen under medical supervision.
Emergency Action Plans for Anaphylaxis
Every child with severe allergies needs an emergency action plan. This plan outlines steps to take during an allergic reaction.
The plan should include:
- Symptoms to watch for
- When to use epinephrine
- Emergency contact numbers
Schools and caregivers should have copies of this plan. They should also know how to use an epinephrine auto-injector.
Regular practice with a trainer auto-injector can help prepare for emergencies. Wearing medical alert jewelry can also inform others about the allergy.
Management of Allergies in School Settings
Schools play a key role in keeping allergic children safe. They need clear plans and rules to handle allergies. This helps protect students and lets them take part in school activities.
Many schools now have “allergy-aware” policies. These rules limit foods that often cause allergies, like peanuts. Some schools ban these foods completely. Others have special tables in the cafeteria for kids with food allergies.
Staff training is very important. Teachers and other workers should know how to spot allergy signs. They also need to learn how to use emergency medicine like EpiPens.
Schools should have action plans for each allergic student. These plans spell out what to do if the child has an allergic reaction. They list the child’s triggers, symptoms, and medicines.
Good communication between parents, doctors, and schools is crucial. Parents should give schools up-to-date info about their child’s allergies. They should also provide any needed medicines.
Schools can take steps to lower allergy risks:
- Clean surfaces often to remove allergens
- Have soap and hand sanitizer available
- Keep rescue medicines in easy-to-reach spots
- Make sure all staff know where medicines are kept
With the right plans and care, schools can be safe places for kids with allergies.
